Introduction Indications for foreign body removal include the following:28 Local anesthesia provides the mainstay in pain control for foreign body removal. Once the patient's neurovascular and functional status have been established, adequate anesthesia and pain medication should be promptly administered. Anesthetics may be administered directly into the wound, topically, or via regional nerve blocks. Proper irrigation is an important factor in reducing the risk of wound infection. No single technique is best for the removal of soft tissue foreign bodies.13,30,45,46,47,48,49,50,51,52,53 Each case must be addressed independently based on the patient’s medical history and the clinical presentation of the wound. The following principles, however, offer a guide: Complications involving soft tissue foreign bodies comprise the following:19,5,22,24,28,56 Radiologic evaluation of soft tissue injuries plays an important role in detecting, evaluating, and planning the potential removal of a foreign body. If clinical suspicion is high, imaging serves as an essential tool in management when no foreign body is found on examination and exploration. When choosing an imaging modality, consider the need for real-time imaging or to evaluate nearby structures, such as vessels, nerves, tendons, and bones. Depending on the modality chosen, important information may be available about the position of the foreign body, nearby structures, and surrounding tissue reactions. It is also important to consider radiation exposure, particularly as ultrasound is a safe, noninvasive, and inexpensive imaging option. History of the injury is particularly important, as the material type of the foreign body may assist in imaging modality selection. Radiography Computed tomography (CT) CT plays an important role in the detection of foreign bodies and the plans for their removal, particularly those that are radiopaque and deeply embedded in the tissue.28,30 CT affords some ability to visualize foreign bodies that are radiolucent on conventional radiographs, though with only intermediate sensitivities.59,60 CT provides more detailed information about local anatomy, tissue reactions, and abscess formation than does radiography or fluoroscopy, and it can more effectively demonstrate foreign body position and orientation. CT is also easily accessible in the emergency department (ED), is more efficient than MRI, and provides substantial information for the resources invested.50 Unlike ultrasound, however, CT is expensive, is associated with significant ionizing radiation, and is not a dynamic modality (ie, cannot provide real-time images for the emergency physician). CT is not routinely recommended to rule out a radiolucent foreign body but can best be used when a foreign body is suspected but not detected by radiographs or ultrasound.61 Magnetic resonance imaging (MRI) MRI is rarely used for foreign body detection during the initial ED visit. However, MRI can provide detailed information regarding tissue inflammatory reactions, osteoblastic or osteolytic changes, and secondary tissue reactions that can aid in determining the presence and location of an otherwise occult foreign body. Certain types of foreign bodies can result in significant artifact on MRI imaging. One particular type of foreign body, gravel, is often ferromagnetic, which causes significant streaking artifact on the MR images.26,50 The use of MRI is limited because of its cost and lack of availability relative to other imaging modalities described. MRI is impractical for routine foreign body detection in the ED but should be considered in cases of longstanding wounds or focal infections with unknown etiology in which the presence of a foreign body is being considered.50,51 Crawford and Matheson used ultrasonography to evaluate 39 patients who had a suspected retained foreign body despite negative soft issue radiographs. In their study, ultrasonography correctly identified 19 of 20 patients with confirmed foreign bodies.47 Friedman and colleagues suggested that ultrasonographic detection of foreign bodies in children, when performed by a pediatric emergency medicine attending, produced results comparable to those produced by plain radiographs interpreted by an attending pediatric radiologist.65 Contraindications to foreign body removal by a nonspecialist involve the following:14,21Introduction
Patients with skin and soft tissue wounds commonly present to the emergency department (ED) for evaluation and treatment. Essential in the evaluation of these wounds is a careful assessment for retained foreign bodies (FB), as they are frequently missed on initial evaluation.1,2 Identification of a foreign body can be difficult, depending on the type and location of the wound and the timing and mechanism of injury. Soft tissue foreign bodies most commonly occur secondary to penetrating or abrasive trauma, and they can result in patient discomfort, deformity, delayed wound healing, localized and systemic infection, and further trauma during attempts at removal.1,3,4 See images below for examples of foreign body presentations.
3-mm hole in patient forearm (entrance).

Author strategy for traumatic nail removal. Cast cutter was used to remove shoe through which nail was embedded. Following placement of a nerve block, the nail was then cut at the surface of the foot with bolt cutter and removed with steady pulling, with remaining nail fragment traveling from plantar to dorsal foot surface.
Missed foreign bodies frequently result in physician malpractice litigation. Wound care is the subject of 5-20% of lawsuit claims against emergency medicine (EM) physicians, resulting in 3-11% of monetary awards.5
History
Assessment of a patient with a suspected foreign body begins with a careful history and physical examination. Patients who present with a wound or localized pain following trauma should be questioned regarding the specific timing and nature of the injury, the level of wound contamination, and any materials involved in the injury (eg, wood splinters, shattered glass, shredded metal). Foreign bodies detected in the ED are most commonly composed of wood, glass, or metal.6 A careful assessment of the patient’s current symptoms should be made, including the location, quality, severity, and radiation of pain; the presence of a foreign body sensation; swelling, warmth, or redness to the wound; and any neurologic symptoms (including motor or sensory deficits).4 Injuries involving the hands mandate asking about hand dominance, patient occupation, and previous hand injuries.
Additional historical information regarding tetanus immunization status, allergies (particularly to local anesthetics, antibiotics, and latex), preexisting medical conditions (eg, diabetes mellitus, HIV/AIDS, chronic renal failure, connective tissue disorders), and medications (eg, steroids) that may influence rates of infection and wound healing should also be noted.1,3,7,8,9,10,11
In most cases, foreign bodies are the result of accidental trauma directly to the skin and soft tissue; these events are usually readily recounted by the patient. However, if the injury resulted from other mechanisms, such as syncope, seizures, potential child or elder abuse, assault, or self-inflicted wounds, further investigation is required.12,13 Cases that involve solid, formed metallic objects obvious on examination (eg, nails, staples, needles) may require a less detailed history than an individual who presents with localized pain and foreign body sensation but is unaware of the timing and exact mechanism of injury (eg, resulting from syncope, seizure, or assault).14
Physical examination
Prior to wound examination, maximize lighting and patient positioning. Physical examination of the affected area should adequately assess for nerve, tendon, vessel, and joint involvement. Perform a vascular assessment focusing on color, capillary refill, and palpation of distal pulses. A neurologic examination should include testing of the surrounding and distally distributed nerves and assessing 2-point discrimination. Evaluate functional status, concentrating on potentially involved muscles, tendons, and joints.1,4 A functional assessment of movement helps to refine the potential musculoskeletal damage that may have occurred during injury and FB deposition.
Providing local anesthetic (ie, digital block) prior to wound inspection and irrigation is essential for patient comfort and in obtaining a more comprehensive examination. Local anesthetics should not be applied prior to careful evaluation and documentation of neurovascular status of the affected area. Foreign bodies such as a nail protruding through a foot may be obvious; however, foreign bodies are more often subtle, such as a small shred of metal imbedded in a fingertip during the opening of a can. If no wound is present, a close visual inspection of the area of localized pain is the first step in determining whether a foreign body is visible. Levine et al demonstrated that 78% of foreign bodies were discovered after physical examination and exploration alone, without the use of imaging.6
To achieve adequate visualization, a hemostatic field of the wound should be established using either direct pressure, a properly placed tourniquet proximal to the wound, or application of newer hemostatic agents such as Gelfoam or QuickClot (Z-Medica Corp, Wallingford, Conn).15,16,17 Note and document wound characteristics, including location, size, color, level of contamination, signs of inflammation (edema, erythema), and presence and type of visible foreign bodies. Obvious skin punctures should not distract the examiner from less obvious areas potentially harboring retained foreign bodies, such as areas where skin may be tenting, edematous, or otherwise normal in appearance. Carefully palpate for a foreign body or a point of maximal tenderness. Palpation of a foreign body may also yield information regarding its exact location, positioning, and orientation, as well as its flexibility and mobility.18
Delayed presentation
Foreign bodies are frequently missed during the initial evaluation, and not all patients present immediately following an injury. In one retrospective study, nearly 38% of patients had foreign bodies that were missed on initial wound inspection.2 Another study found that only 75% of soft tissue foreign bodies were presented within 48 hours, while patients with the remaining 25% presented weeks, months, and even years later.6 Additional reports have demonstrated subcutaneous soft tissue foreign bodies from splinters to bullet fragments found years after the traumatic event (eg, gunshot wound).19,20,21,22,23,24,25,26 Delayed foreign bodies can present as localized cellulitis, abscess, or regional inflammatory response. A history of recurrent localized infections should prompt a search for an occult foreign body and should include a discussion of recent or remote trauma that could have resulted in a foreign body.18,20,21,27Indications
The potential for complications due to the process of foreign body removal must be considered. Such complications may include the following:27 Anesthesia
Equipment
Positioning
Technique

Placement of ankle nerve block for traumatic nail removal.

Nail embedded in the foot, propelled by nail gun through soft tissue and bone.

Patient's foot following nail removal. The patient suffered no acute complications.
Pearls
Complications
The patient should be informed of the potential for these complications at every step. Document that the patient received this information; adequate documentation may be useful in the event of a poor outcome.13Imaging
The following 5 imaging modalities are used in foreign body removal:29
Radiographs are considered an adjunct to visual inspection and are often an integral part of foreign body evaluation. They are noninvasive, inexpensive, widely available, easy to interpret, and they can provide positional information (although not in real time) to aid in foreign body removal.29,30,57,58 See images below.
Anteroposterior radiograph depicting foreign body projectile fragments in a patient's forearm.

Lateral radiograph depicting foreign body projectile fragments in a patient's forearm.

Anteroposterior (panel A) and lateral (panel B) radiographs of the left index finger demonstrating a nail embedded in the distal phalanx following a nail gun injury.
Radiographs are most useful in detecting radiopaque foreign bodies with sensitivities above 95% with adequate penetration and multiple views (anteroposterior and lateral).29,30,45 However, for the detection of nonradiopaque foreign bodies (eg, wood, rubber, plastic, and other plant-based foreign bodies), the sensitivity of radiography is low.30,45,46,57 One randomized blinded study showed a sensitivity of only 5%.6 In a retrospective case series reviewing 490 cases of foreign bodies, Levine and colleagues reported that radiographs were ordered 50% of the time and had a sensitivity of nearly 100% for the detection of metal but missed 93% of wood and 25% of glass foreign bodies.6
If appropriate radiolucent surface markers are used prior to the radiograph (ie, 2 surface paper clips, one in the anteroposterior and the other in the lateral plane), positional information of the foreign body relative to the surface markers can be used if retrieval is planned.47,48 At least 2 radiographic views (ie, anteroposterior and lateral) are likely sufficient in most cases for adequate foreign body localization. Radiographs can also provide detailed information on the potential number of foreign bodies present (and their absolute or relative sizes), which can be used when determining appropriate irrigation, exploration techniques, and the need for postprocedure antibiotic prophylaxis.
Fluoroscopy
Fluoroscopy can be useful in foreign body removal if a C-arm or other appropriate imaging equipment is accessible. This technique allows for real-time radiographic visualization of the foreign body and affords the clinician the opportunity to precisely locate the foreign body using skin markers. A technique has been reported in which, after a local field block, 2 small needles were placed and advanced into the skin at perpendicular angles under fluoroscopy until they were both touching the foreign body. An incision was then made to connect the 2 needles, and foreign body removal was readily achieved using blunt dissection.47
Ultrasonography
The use of bedside ultrasonography to detect and localize soft tissue foreign bodies in the ED is gaining in acceptance and popularity because of its ease of use, increased availability, lack of radiation exposure, safety, and sensitivity with detection of certain types of foreign bodies.48,52,53,55 See images below.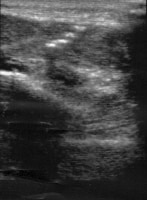
Ultrasound of projectile foreign body fragments in a patient's forearm.
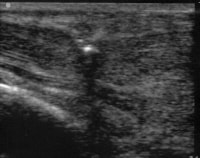
Ultrasonographic guidance (active) of retrieval of projectile foreign body fragments in patient forearm. Note tissue tenting at tip of forceps used to retrieve the most superficial fragment.
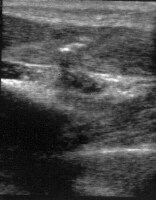
Ultrasound of remaining projectile foreign body fragments in patient forearm after active ultrasound-guided removal of the most superficial fragment.
Ultrasonography affords the clinician real-time localization of foreign bodies and can also yield diagnostic information regarding the presence of soft tissue edema or abscess formation.32 The technique involves using a linear ultrasound probe and placing a fluid-filled bladder (eg, saline-filled latex glove) between the linear probe and the skin (with appropriate lubrication on both), or using a small pad on the skin to allow for transmission of ultrasound waves and improved field of view.48,52 Foreign bodies are demonstrated as hyperechoic foci with shadows that depend upon the foreign body size and composition. Hyperechoic halos provide evidence of soft tissue inflammation or edema but can also indicate abscess or granulation tissue.52 Because of their higher material densities, metallic or radiopaque foreign bodies often cause hyperechoic comet-tail artifacts.32
Ultrasound-guided foreign body removal reduces procedural time and morbidity and improves time to detection and procedural outcomes.25,48,52 However, using ultrasonography to detect foreign bodies is operator-dependent and often difficult to interpret; its utility varies depending on the type of foreign body. While initial reports have demonstrated sensitivity rates below 50% for ultrasound detection of gravel, metal, wood, glass, and plastic, more recent reports have described improved sensitivities.62,63 Much of the clinical data supporting ultrasound use in the detection of foreign bodies has been in the form of case reports and nonclinical studies.58,62 In a randomized blinded study using ultrasonography to detect foreign bodies in a chicken thigh model, Turkcuer and colleagues reported a sensitivity of 90% for identifying nonradiopaque foreign bodies, such as wood and rubber.62
Data in humans support the use of ultrasonography for soft tissue foreign body removal. Gilbert and colleagues demonstrated that ultrasonography could identify 21 of 22 foreign bodies in 50 patients suspected of having a radiolucent foreign body.63 In a prospective study of 45 patients in whom both radiographs and ultrasounds were used for detection of a foreign body, Banerjee and Das demonstrated that ultrasonography could detect radiopaque foreign bodies in 19 of 20 patients in whom radiography detected foreign bodies and could identify foreign bodies in 7 of 25 patients whose radiographs demonstrated negative findings.64
The American College of Emergency Physicians (ACEP) 2009 Emergency Ultrasound Guidelines recognize foreign body detection and removal as a unique and evolving application of emergency ultrasound.66 Given the sensitivity (and lack of sensitivity of other imaging modalities), advantages of real time evaluation, accessibility, lack of radiation, and noninvasive nature, high-resolution ultrasonography has become the main imaging tool used for the detection and localization of nonradiopaque foreign bodies in soft tissueContraindications
Saturday, November 27, 2010
Labels: Foreign Body Removal, Wound
Subscribe to:
Post Comments (Atom)
0 comments:
Post a Comment